Venous thrombosis is a condition that requires urgent medical intervention when it occurs. In this article, Dr. Fareed Al-Adham answers the question of what venous thrombosis is, and how it is diagnosed and treated.
What is Venous Thrombosis?
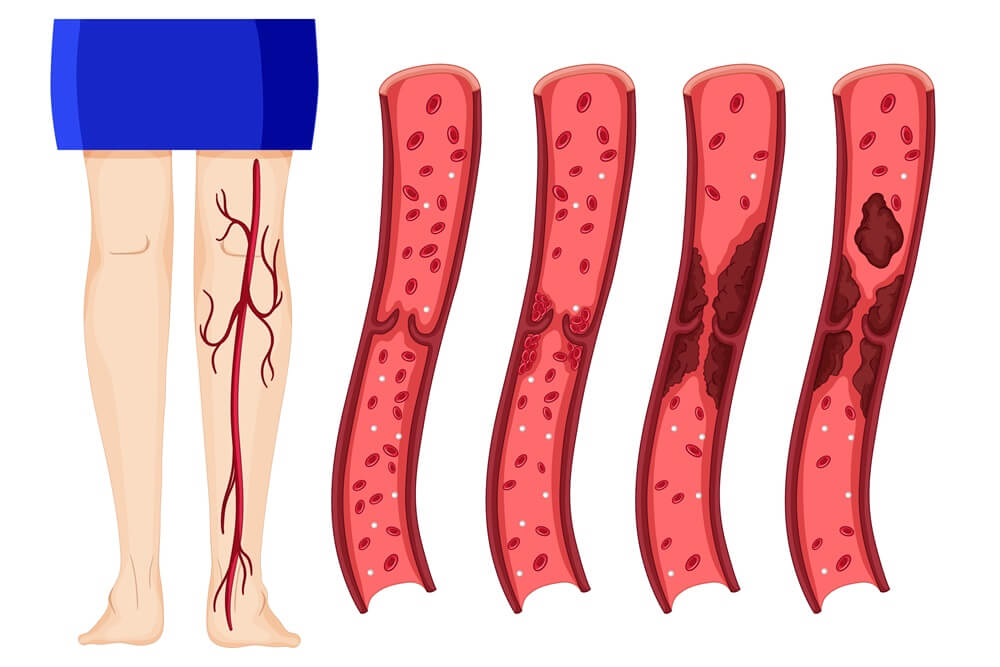
Venous thrombosis is a medical condition characterized by the formation of a blood clot in one of the veins, often occurring in deep veins in the leg or arm, known as deep vein thrombosis (DVT).
The blood clot leads to stagnation of blood in the area preceding the blockage, depriving cells and tissues downstream of oxygen. The clot may then travel through the body's veins to one of the pulmonary blood vessels, causing obstruction, known as pulmonary embolism.
Causes of Venous Thrombosis
The occurrence of venous thrombosis is attributed to two main factors:
-
Damage to the walls of deep veins, which can occur during certain surgeries, direct injury, inflammation, or infection, leading to disruption of blood flow through the veins.
-
Genetic blood clotting disorders, such as hereditary thrombophilia, which disrupts the proteins responsible for blood clotting, making individuals more susceptible to venous thrombosis.
Risk Factors for Venous Thrombosis
The likelihood of developing venous thrombosis increases in the following cases:
-
Venous injury, such as fractures, severe muscle injuries, and major surgeries, especially abdominal, pelvic, and leg surgeries.
-
Prolonged immobility, causing sluggish blood flow through the veins due to factors like bed rest after major surgeries or paralysis.
-
Hormonal therapies, which raise estrogen levels, such as in women using birth control pills or hormone replacement therapy after menopause.
-
Pregnant women, with the risk persisting for up to three months after childbirth.
-
Personal or family history of venous thrombosis, increasing the risk for individuals who or whose family members have had a previous clot.
-
Other medical conditions, including certain blood disorders, cancers, heart diseases, inflammatory bowel disease, or diabetes.
-
Unhealthy lifestyle habits, particularly among smokers, obese individuals, and those with sedentary lifestyles.
-
Personal factors such as age and gender, with the risk doubling every ten years after age forty and higher risk for women compared to men before menopause, while decreasing after menopause.
Symptoms of Venous Thrombosis
Venous thrombosis leads to symptoms in the area of venous obstruction, whether in the lower or upper limb. When a blood clot detaches and travels to the lungs, it may cause additional symptoms in the chest. The symptoms of venous thrombosis include:
Symptoms of leg or arm thrombosis:
-
Swelling and pain in the affected leg or arm.
-
Redness or bluish discoloration of the skin in the affected area.
-
Increased temperature in the affected area compared to neighboring areas, with warmth felt upon touch.
Symptoms of pulmonary embolism:
-
Sudden shortness of breath.
-
Severe chest pain, worsened by deep breathing.
-
Rapid heart rate.
-
Coughing up blood in some cases.
Diagnosis of Venous Thrombosis
Diagnosing venous thrombosis is done through imaging of blood vessels using ultrasound (sonar) to detect blood flow through the veins, or by CT angiography to diagnose pulmonary embolism.
Typically, the doctor performs these tests after taking the medical history, examining symptoms, and conducting a clinical examination. Additional tests may be required for a more accurate assessment of the condition and to rule out other similar conditions. These tests may include:
-
D-dimer test, which measures the level of a substance produced by the body in the blood when a blood clot detaches from its site.
-
Contrast venography, where veins are imaged using X-rays after injecting a dye into a major vein in the foot, is the most accurate diagnostic method.
-
MRI or CT scans.
Treatment of Venous Thrombosis
Once venous thrombosis is diagnosed, treatment should commence immediately to control the condition, reduce the size of the clot, and minimize the risk of detachment and migration to the lungs or occurrence of another venous thrombosis. Treatment methods include:
Medical treatment
Administering anticoagulants orally, intravenously, or subcutaneously, with doctors often prescribing one type of heparin for 5 to 10 days, followed by oral anticoagulants for 3 to 12 months after the patient recovers.
IVC Filter Placement
Placing a filter in the vein that returns blood from the lower extremities to the heart (the inferior vena cava) allows blood to flow around the venous thrombosis, preventing its transfer to the lungs. This method is used when medical treatment is contraindicated.
Venous Thrombolysis
This option is often chosen for severe cases of venous thrombosis. It is a simple surgical procedure where a small tube is inserted into one of the leg veins, guided by ultrasound and X-rays to reach the site of blockage, where medications are injected to dissolve the blood clot.
Additionally, doctors recommend that patients with venous thrombosis wear compression stockings that cover the foot and leg, as they help prevent blood stagnation in the leg veins and reduce leg swelling.
Prevention of Venous Thrombosis
The risk of developing venous thrombosis can be reduced by following these recommendations:
-
Maintain a healthy weight.
-
Exercise regularly.
-
Drink adequate amounts of water throughout the day.
-
Avoid prolonged immobility.
-
Avoid sitting with crossed legs, especially for extended periods.
-
Quit smoking.
-
Avoid alcoholic beverages.
